(9 pm. – promoted by ek hornbeck)
Lyme Disease is a new condition in our infectious disease panoply. It has only been suspected since 1975, and only in 1978 was it suspected to transmitted by ticks. The causative agent was not identified until 1981. This piece is intended only to be a very basic survey of the condition and some of the controversies surrounding it, not a comprehensive dissertation. There is a very good group at Dailykos called Lyme Disease Awareness with contributors who have more personal information than I do. If you’re worried that you have the condition, there is a lyme disease dna test you can take that will give you a realistic diagnosis, don’t depend on this article as an alternative. Do not take anything you read in this piece or in the group in general as a substitute for competent medical advice and treatment. If you require some more comprehensive support and suspect you might have a reaction from lyme talk to a professional from the Holtorf Medical Group or a similar medical professional.
Let us think about that for a minute. Western medicine had recognized most all serious infectious diseases since the time of Herodotus! Certainly some exceptions are present, such as syphilis, with seems to be a New World import to Europe and certain, very long latent period virus diseases that we are just now discovering.
Lyme Disease is different, though. It is caused by a bacterial agent, a specific spirochete called Borrelia burgdorferi, the species name from its discoverer, the brilliant Swiss-American biologist, Dr. Willy Burgdorfer.
Dr. Burgdorfer “cut his teeth” on a spirochete of the genus Borrelia, a singularly nasty genus. Dr. Burgdorfer originally studied Borrelia duttonii, the causative agent for African relapsing fever, oddly enough also with a species of tick as its vector. This infection is also endemic in the western United States and Canada, but is not a huge public health issue because it is rare.
On the other hand, Lyme Disease is likely more common than we would like to think. I truly believe that it contributed to the death of my mum, so I have sort of a personal stake in it, but hope not to let that cloud my scientific judgment about the facts and the hype in this piece.
This condition is named for Lyme, CT, where it was initially suspected as being a previously unknown infectious disease in 1975. There are a couple of different species of the spirochete that cause similar maladies in Europe, so it is not a uniquely North American infection as I speculated in a reply to a blog Thursday. It is not something that you want to get.
Spirochetes (“spiral bacteria”), along with cocci (spherical ones) and bacilli (sort of rod shaped ones), cause many diseases in plant, animals and humans. There are lots of gradations insofar as their shape goes, so the three that have chosen are not necessarily all inclusive. These three groups are from classical bacteriology, and modern studies have identified many intermediate kinds, and some that are well described within these terms. Interestingly, some of these bacteria are essential for life as we know it, but I am not aware of any spirochete that is beneficial.
In any event, this bacterium is fairly easily transferred from tick to human, with a horrible toll in many cases. The life cycle is complex, but the important causes of human infection boil down to deer, ticks, and humans. We humans are just unfortunate victims of the infection, because the life cycle of the bacterium is fine only with ticks and deer.
In North America, the vectors for transmission are pretty much ticks (most of the genus Ixodes) that are hard bodied. Soft, “dog ticks” are not often implicated. One species, Ixodes scapularis, also called the Deer Tick or the Blacklegged Tick, is most at fault, at least in the eastern part of the United States. I have not seen many of them from my ancestral home, western central Arkansas, but a really common one there is the Spotted Tick, Amblyomma americanum. Studies show that it is less likely to be a viable vector of the spirochete, but I can assure you that there are LOTS of Spotted Ticks in my ancestral home.
In any event, the spirochete is happy in its host, the White Tailed Deer Odocoileus virginianus, a cervid also under suspicion for being a natural host for Bovine Spongiform Encephalopathy, also called BSE or Mad Cow Disease. Interestingly, the deer population has become extremely large these days compared to those 80 years ago, mostly because of restoration of forest habitat and lack of hunting, but that shall be discussed later.
In an environment without people, the hard ticks infest the deer and inject the spirochete into them. Apparently the spirochetes do little damage in deer, but one has to realize that deer live only for a decade or so, except in rare individuals, so the long term sequelae of the infection are probably not manifested like they are in humans. In the real world, those baby (and adult) ticks eat their fill on blood and drop off of the deer, and then climb up tall grass and weeds, waiting for a new host to approach. Then, feeling the motion, they drop off of the plant and, if lucky, latch onto a new victim.
Unfortunately, sometimes those victims are people, who seem to have a bizarre nondefensive reaction to them. Most folks think of deer, but according to the National Institute of Allergy and Infectious Diseases, rodents are actually the main reservoir in nature. It does not matter how your tick got infected. When the tick penetrates the skin of a human, bad things happen, even if the tick is not infected. I say “penetrate”, because they have something like a hypodermic needle (but constructed in such a manner that it is not easy to remove) rather than proper mandibles (aka jaws). The tick literally pushes its proboscis into the body, and then starts to feed, by taking blood (the mother’s milk for a tick) and also adding a very interesting material to the wound.
It turns out, at least for the Deer Tick, that its saliva has a compound in it that actually suppresses the human immune system, at least locally, allowing the spirochetes to reproduce at a very high rate. This is not good.
In “classic” cases, a peculiar rash, called Erythema migrans (EM) or “bull’s-eye” rash. According to CDC, this is present in 70 to 80 % of new infections, but some researchers use a much lower figure, maybe around 30 to 40 %. This rash typically presents in a week or two, but may form in as soon as three days or be delayed for 30 or more days, and obviously sometimes NEVER develops. Here is a picture of the classic rash.

Erythema migrans
During the time of the rash, additional ones may or may not develop Also, neurological symptoms may also develop, such as Bell’s palsy (a drooping of the facial muscles), severe headaches, and even meningitis. Inflammation of the large joints may also occur, as well as changes in heart rhythm. Some, all, or none of these symptoms may present, making Lyme Disease difficult to diagnose.

Bell’s Palsy
Left untreated, CDC estimates that the majority of patients will develop arthritis, particularly of the knees and a minority will develop chronic neurological complications in the month to years timeframe. Some of these conditions may be irreversible, so if you think that you might have Lyme disease, seek medical treatment fast. But the news sort of gets worse.
Even in patients treated successfully with antibiotics, CDC estimates that up to 20% will continue to present symptoms even though the initial infection is cleared. Joint and muscle pain are frequent in these patients, as well as cognitive disorders, chronic fatigue, and sleep disturbances, which may be related to the fatigue. Here is where things get quite controversial.
There are a group of physicians and laypeople who insist that the treatment lies with continued, long term use of antibiotics, although no credible study has shown that to be the case. The cause is actually thought to be, but this is also controversial, a disruption in the manner in which the immune system operates, so the Post Treatment Lyme Disease Syndrome (PTLDS) may actually be an autoimmune disease caused by the infection permanently causing the immune system to recognize the patient’s own cells as invaders.
Now, in my limited research I have not seen this discussed: IF PTLDS is an autoimmune reaction, treatment with gluticocortical steroids should provide some relief by partially suppressing the the immune system to some extent. Now, do not get me wrong: I am not a big fan of long term steroid therapy, but long term antibiotic therapy is pretty undesirable too. CDC insists that the long term antibiotic therapy does not help, so perhaps it would be instructive to try some prednisone in a few patients with severe symptoms and see it IT helps. If not, it can be discontinued after a couple of weeks (it usually works pretty fast in other maladies) with no long term damage. It seems to me a simple experiment to try, and steroids are cheap.
The most important single approach to attacking Lyme Disease is prevention, and that can easily be done by individuals, even without any particular training. One of the most important is to use repellents to discourage ticks from attaching. Some authorities recommend long sleeves and pants, with boots when walking in areas where Deer Ticks are common. In a bit I shall show a map of their area. I would add to the boots and long pants duct tape, to seal the cuff of the pants to the boots.
After visiting an area where ticks are present, a thorough examination of the skin and scalp should be made, and any ticks removed (using tweezers right at skin level) promptly. Studies indicate that it takes from 24 to 36 hours for the tick to begin to release the spirochete into the wound. This makes sense, because at the beginning of the bite, the tick is intent on taking up as much blood as possible, so a gradient is formed where the flow is pretty much into the tick. As it becomes engorged, it does not suck as hard, allowing its gut contents to infiltrate into the wound. After tick removal, use soap and water to disinfect the area around the bite, the tweezers, and the hands. Pay special attention to areas that tend to chafe, like where a belt is drawn, and hard to see areas. Those with significant others have an advantage here, but a hand mirror will work.
Back on the old days when people worked in the fields and woods, the nightly ritual was to search for ticks carefully and remove them. Those people may have taken only a weekly bath, but they were serious about ticks. Here is a map of the high risk regions in the United States.
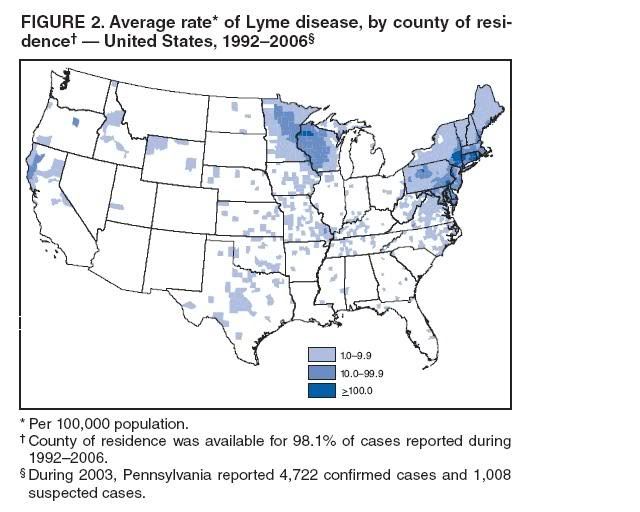
High Risk Regions
Here is a simple graphic for the life cycle of ticks, and note that probability is highest in the summer, when most the ticks are in the nymph stage, about the size of a poppy seed.
Tick Life Cycle
Here are pictures of several species of ticks during the life cycle.
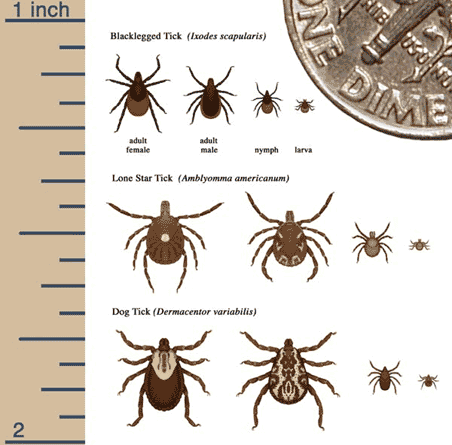
Tick Pictures
If you do see an EM form, you need to get the the doctor right away. If you still have the tick, bring it with you. The problem is that there is not a good blood test for Lyme, at least in its early stages. Only after a significant infection has developed are enough antibodies formed to cause the ELISA Enzyme Linked Immunosorbent Assay and Western Blot tests to show a positive. Studies show that the urine based tests are quite unreliable, often giving false positives, whilst the combination of ELISA and Western Blot have an accuracy approaching 100%. You do not want to be treated with heavy antibiotics if you do not need them.
We are not at the day yet when a test is available for direct detection of Borrelia burgdorferi by its DNA is available for widespread use. This would be the way to go, because people with previously cured infections of Lyme still can give positive antibody tests, because antibodies stay around a long time. If Lyme DNA could be the target for the test, then it would remove that limitation.
The current guidelines for treating Lyme can be summarized thus:
Only people with early symptoms should be treated except in rare circumstances when antibiotics can be used to prevent it.
The drug of choice is doxycycline for 14 days. If a patient can not take this drug, either amoxicillin or cefuroxime can be used. Pregnant and nursing women should avoid doxycycline, and also children under eight.
If it has not been caught early, then more aggressive treatment is necessary. IV ceftriaxone in large doses for two weeks is the standard, but alternates are injected cefotaxime or penicillin G. A longer oral regimen of doxycycline has also been found to be effective, since it is effective orally, but again, young children and lactating and pregnant women should not use this drug.
For late stage Lyme, the treatments are more aggressive yet. The same drugs as for early stage disease are used, but for 28 days, and another 28 day regimen may be necessary. The problem is that, as I mentioned earlier, the longer the disease is present the less effective treatment becomes.
For the chronic condition, there is really no good treatment, partially because there is no evidence for bacteria being present after heavy antibiotic protocols. That makes treatment extremely difficult, and some authorities have suggested that there may be some psychosomatic involvement, whilst others, and I said earlier, think that an autoimmune component is present. This remains to be resolved, and other than my steroid hypothesis, I see no really good trends at present. Of one thing I am pretty sure: not all of the symptoms are psychosomatic. One thing often overlooked is that some patients may be suffering from unrelated conditions that mimic those of Lyme, like multiple sclerosis and other neurological conditions, but have associated their conditions with the Lyme that was cured long ago. Remember, there are lots of causes for fatigue, muscle and joint problems, and neurological deficits. This area requires much more research.
Well, you have done it again! You have wasted many more einsteins of photons reading this sour piece. And even though Newt Gingrich forgets that his master is Rush Limbaugh when he reads me say this, I always learn much more than I could ever hope to teach by writing this series, so keep those comments, questions, corrections, and other feedback coming. The comments are the best part of this series! Remember, no science or technology related thought is off topic here. Tips and recs are also very welcome. I shall stick around tonight as long as comments warrant, and shall return tomorrow about the same time for Review Time.
Warmest regards,
Doc

2 comments
Author
trying not to get this condition?
Warmest regards,
Doc
Author
I very much appreciate it.
Warmest regards,
Doc